Originally published on Psych Central
https://blogs.psychcentral.com/triple-winner/2017/03/the-stigma-of-co-occurring-disorders/
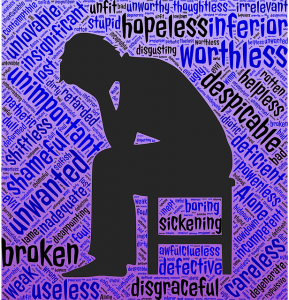
There is a great deal of stigma attached with both mental illnesses and addictions. That is one reason I talk about my experiences. So, others won’t feel alone, and, to put a face to these conditions. It is scary to get a diagnosis of a life-long mental health condition that all you have heard are extreme negatives. People can lose hope. And, people fear what they don’t know.
I also have shame, or self-stigma. I have worked on accepting the schizoaffective diagnosis and at this point am okay. There was a time when I felt, less than, because of the severe symptoms. Now, I know I could not control what happened in the past, and just work on staying stable.
Social anxiety is something I contend with daily, and I cannot seem to prepare enough. I don’t know if I can ever accept how limiting it is for me. There are some things, like volunteering at my children’s school events, that are just too busy for me. I cannot enjoy shopping or parties, I just want an exit. I have worked very hard on this and work with people now and even do public speaking, but it is difficult.
The alcohol addiction label is new to me. In the program I am doing, SMART Recovery, they don’t give labels. But, I need to call it something. The drinking is not new, just the acknowledgement.
There are choices of programs for changing addictive behaviors. Some people work more than one at a time. This was just one that seems to fit my philosophy. It uses cognitive behavioral therapy (CBT) principles and I already learned some of those for my anxiety.
I haven’t had serious consequences from drinking. No DUIs or jail time, No relationship problems. But, I drink more than I would like and it is hard for me to abstain completely.
I decided I would like to write about the alcohol component along with the mental illness. So many of us have co-occurring disorders. I was excited, and then, I paused. What will people I know think when they see ‘alcoholic’?
I couldn’t decide which was the worst of 2 stigmas. It doesn’t matter.
Info on SMART Recovery
http://www.smartrecovery.org/
Info on Alcoholics Anonymous (AA)
http://www.aa.org/